Chronic Plantar Fasciitis

Plantar fasciitis is a common reason for long-lasting heel pain. It can affect both active, young people and older people who do not move as much. This condition happens when the plantar fascia, a band of tissue in the foot, is repeatedly strained. It is often linked to tight calf muscles. Podiatrists can generally diagnose this condition by talking to the patient and examining their foot. They only use imaging tests if the case is unusual or does not get better with initial treatment. The main symptom is a sore heel, especially when taking the first steps in the morning or after sitting for a while. Treatment involves changing activities and stretching the calf and foot. Special shoe inserts that support and cushion the heel can also help. If pain continues after six months, podiatrists may suggest less invasive treatments or even surgery. These treatments help the body heal itself or relieve pain. However, some injections, while they reduce pain, could also weaken the foot tissue. Surgery options involve releasing tension in the calf or making small cuts in the plantar fascia to encourage healing. If you have chronic plantar fasciitis, it is suggested that you make an appointment with a podiatrist who can determine what the best treatment options are for you.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Jennifer M. Kern, DPM from South Carolina. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in West Columbia, SC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
How Aging Can Affect Your Feet

As time passes, the body undergoes natural changes, and our feet are no exception. Subjected to a lifetime of impact, weight-bearing and pressure, your feet gradually transform, affecting their strength and resilience. One noticeable change brought on by aging is the thinning of the skin, reducing natural cushioning and making the feet more vulnerable to damage. Joints in the feet undergo wear and tear, leading to conditions like osteoarthritis. Joints become less flexible, causing the foot to lose its springiness and ability to absorb impact. Muscle strength, which peaked in your 20s and early 30s, gradually diminishes with age. Regular exercise slows this decline and helps to maintain overall foot health. Swelling, a common issue with age, increases pressure on the foot's structures. Poor circulation, often associated with conditions such as atherosclerosis, affects the blood supply to the feet and reduces their ability to repair minor injuries quickly. Toenails also undergo changes, becoming thicker and more brittle as growth slows. Conditions like hypothyroidism and peripheral arterial disease can make this worse. For help in managing foot problems associated with aging, it is suggested that you make an appointment with a podiatrist.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact Jennifer M. Kern, DPM from South Carolina. Our doctor can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in West Columbia, SC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Elderly and their Feet
While proper foot care is important for everybody, senior citizens have the tendency to be more susceptible to certain foot conditions. The elderly should therefore be well informed about any problems that may arise and about what they can do to properly avoid or treat them.
Some of the most common foot problems seniors are susceptible to include foot ulcers, ingrown toenails, fallen arches, and fungal nails. A foot ulcer is an open sore on the foot and can be a result of diabetes and decreased sensation in the feet. An ingrown toenail is defined as when the nail grows into the side of the toe. Fallen arches are indicated by the instep of the foot collapsing. A fungal nails is a condition that results in deformed and discolored toenails.
In order to avoid these conditions it is recommended that the feet be inspected by the patient on a regular basis. If these inspections are carried out routinely, there is a good likelihood that problems can be identified before they become severe, or can even be avoided altogether. If any abnormality is discovered, it is important that the individual consult a podiatrist for diagnosis and information on treatment options.
Proper foot hygiene is also important. Making sure that you always have clean, dry socks on can be a major deterrent to many different problems including bacterial infections, foot odor, and certain types of fungus. Wet feet are a major cause of many of these problems. If your socks get wet, it is important to change them. Walking around in wet socks may not only lead to various infections, but can irritate the skin and result in a number of various complications. Clean, dry feet are less likely to be affected by fungal and other infections.
As people age, the fat present on your feet begins to deteriorate. The protective nature of this fat keeps the feet healthy by providing a barrier between your bones and the ground. This also aids in giving the skin on the feet a certain amount of elasticity. This is one factor that causes elderly people to develop some serious foot issues. Foot moisturizers can be helpful to avoid certain problems associated with this. However, water-based moisturizers do not work as well for elderly people as they do for the young. Instead, it is more effective to use an emollient instead. An emollient is effective because it binds the water in the foot, keeping it from becoming absorbed too readily which will result in dry skin. Emollients also have a special property called occlusion, which provides a layer of oil on the skin. This layer prevents the foot from drying up and can be very effective in treating dry skin disorders. If you can keep the skin on your feet healthy, this will substantially reduce the number of foot problems you will encounter in old age.
Proper footwear is another way to keep feet healthy. Shoes that fit well and provide proper support help prevent ingrown toenails and fallen arches.
Certain medical conditions such as diabetes or poor blood circulation increase the risk for foot issues. For individuals with any of these conditions it is extremely important to conduct regular foot inspections to make sure that there are no sores or infections present.
Managing Chronic Wounds

Chronic wounds on the lower legs, feet, and toes demand a specialized approach from podiatrists to ensure optimal healing. The process begins with cleaning of the wound and removing any debris. In cases of traumatic injury, a podiatrist may recommend a tetanus vaccination to prioritize your safety. This foot doctor may surgically remove dead skin and close wounds with stitches or staples. Dressing choices for chronic wounds are critical, often leaning toward moist dressings tailored to specific wound characteristics. Vigilant monitoring for signs of infection is a key responsibility, with prescribed antibiotics and antimicrobial dressings essential for effective control. A thorough review of patient medications and adjusting as needed, is essential for patient safety. Specific wounds like ulcers may require specialized treatments, including antibiotics or skin grafts. In cases where poor blood supply hampers healing, a podiatrist may recommend vascular surgery to improve circulation. If you are experiencing chronic foot wounds, it is suggested that you schedule an appointment with a podiatrist for a comprehensive treatment plan.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Jennifer M. Kern, DPM from South Carolina. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in West Columbia, SC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Warning Signs From Your Feet

The condition of your feet can offer valuable insights into your overall health. For instance, if your feet are persistently cold, it may signal hypothyroidism, a condition that slows your metabolism. Yellow toenails may be a sign of lymphedema or respiratory issues. Persistent yellowing warrants a visit to a podiatrist for a diagnosis and treatment options. Painful foot cramps can result from dehydration or nutrient deficiencies. It is a good idea to stay hydrated, maintain a balanced diet, and consider drinking low-calorie sports drinks with electrolytes to prevent and relieve foot cramps. An enlarged, painful big toe may indicate gout. This is a form of arthritis that often affects the big toe. It results from an overabundance of purines in the system and can cause flare ups of extreme pain, swelling, and redness in the big toe. Reducing the risk of gout involves moderating alcohol intake and avoiding red meat and seafood consumption. If you are experiencing unusual types of foot problems, or suspect you may have gout, it is suggested that you make an appointment with a podiatrist for a full diagnosis and treatment options.
Everyday foot care is very important to prevent infection and other foot ailments. If you need your feet checked, contact Jennifer M. Kern, DPM from South Carolina. Our doctor can provide the care you need to keep you pain-free and on your feet.
Everyday Foot Care
Often, people take care of their bodies, face and hair more so than they do for their feet. But the feet are a very important aspect of our bodies, and one that we should pay more attention to. Without our feet, we would not be able to perform most daily tasks.
It is best to check your feet regularly to make sure there are no new bruises or cuts that you may not have noticed before. For dry feet, moisturizer can easily be a remedy and can be applied as often as necessary to the affected areas. Wearing shoes that fit well can also help you maintain good foot health, as well as making it easier to walk and do daily activities without the stress or pain of ill-fitting shoes, high heels, or even flip flops. Wearing clean socks with closed shoes is important to ensure that sweat and bacteria do not accumulate within the shoe. Clean socks help to prevent Athlete’s foot, fungi problems, bad odors, and can absorb sweat.
If you have any questions please feel free to contact our office located in West Columbia, SC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Every Day Foot Care
Our feet are important in our everyday lives. The problem is that we tend to neglect them. When this becomes a habit, it can cause significant trouble. Ignoring foot problems can mean pain, limited mobility, and expensive doctor's visits. On the other hand, if feet are cared for and looked after regularly, they will perform without pain or complication.
Routine hygiene is the most basic way to care for the feet. Wash and dry them thoroughly daily. Remember to get between the toes and keep the toenails trimmed and short. If the feet feel dry or there are signs of dryness or cracking, use a moisturizer designed for the feet.
When using moisturizer on the feet, try to avoid applying between the toes. If cream or lotion sits too long, they can cause fungal and bacterial growth. When moisturizer is used between the toes, it can also cause the skin to soften too much.
Shoes are also an important aspect of foot care. When one is picking out shoes, make sure they are the correct size. Shoes need to be snug, but not too tight. On the other hand, if shoes are too loose they can cause foot problems as well. It is highly recommended that shopping for new shoes be done later in the day. The reason for this is that the feet will have settled and swelled to their full size by then. To keep your feet at their most healthy, avoid wearing high heels or flip flops too often. Instead, choose shoes that are good for your feet. Good shoes pad the soles of your feet and support the arches and ankles.
Socks should also be worn daily with closed-toe shoes. They may feel hot during the summer months, but they absorb sweat and moisture off the feet. Without socks, the build-up of sweat in a closed-toe shoe can cause fungal problems and athlete's foot.
The best thing to remember in every day foot care is that shoes do make a difference. If you spend a lot of time on your feet, make sure that your shoes show no signs of wear. Shoes should offer ample support for the arches and the overall foot. Additionally, try to make foot cleaning and maintenance a daily habit. If you keep these things in mind, your feet will stay healthy and safe.
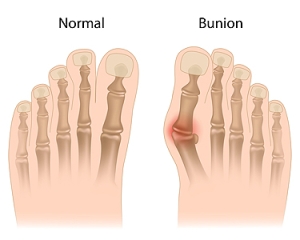
Bunion Complications
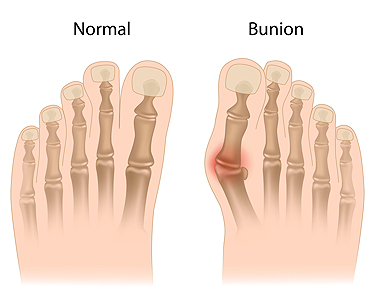
A bunion, medically termed hallux valgus, is a prominent, bony protrusion at the base of the big toe. Often, the only indicator of a mild bunion is its physical manifestation. However, it can also result in discomfort, swelling, and alterations in the foot's structure. In extreme instances, surgical intervention might be necessary due to related issues. Key visual indicators of a bunion are the big toe deviating toward the other toes, forming an outward bulge on the first foot bone. Additionally, there may be a raised bony bump on the foot's exterior, tough skin under the big toe, and calluses on the adjacent toe. Over time, the foot's form may drastically change, impacting both the big toe and other foot regions, making shoe selection challenging. Resulting structural modifications can cause pain, swelling, and bursitis, which is an inflammation of the toe joint's cushioning sac. Some people may face mobility issues with their big toe, affecting their walking. While many individuals do not encounter severe problems from bunions, if left untreated, complications such as arthritis in the big toe or deformities in the adjacent toe can arise. If you have a painful bunion, it is suggested that you make an appointment with a podiatrist who can intervene and help prevent severe complications.
If you are suffering from bunion pain, contact Jennifer M. Kern, DPM of South Carolina. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in West Columbia, SC . We offer the newest diagnostic and treatment technologies for all your foot care needs.